Fetal growth restriction
Fetal growth restriction (FGR), also known as intrauterine growth restriction (IUGR), is a condition where a baby does not grow to its expected size during pregnancy. This condition affects approximately 3-7% of pregnancies and is a significant cause of perinatal morbidity and mortality. Understanding FGR, its causes, diagnostic methods, management strategies, and potential outcomes is crucial for healthcare providers and expectant parents. This comprehensive guide explores FGR in detail, providing actionable insights and evidence-based information.
What is Fetal Growth Restriction?
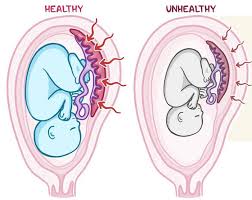
Fetal growth restriction occurs when a fetus fails to achieve its genetically determined growth potential. Doctors typically diagnose FGR when the estimated fetal weight falls below the 10th percentile for gestational age. However, not all small babies have FGR; some are constitutionally small but healthy. FGR is distinct from small-for-gestational-age (SGA), as it implies a pathological restriction of growth rather than a normal variation.
Causes of Fetal Growth Restriction
1. Maternal Factors
- Chronic Health Conditions: Hypertension, diabetes, kidney disease, and autoimmune disorders can impair placental function, reducing nutrient and oxygen supply to the fetus.
- Infections: Infections like cytomegalovirus, toxoplasmosis, and syphilis can directly affect fetal growth.
- Lifestyle Factors: Smoking, alcohol consumption, and drug use significantly increase the risk of FGR.
- Poor Nutrition: Inadequate maternal nutrition, especially in low-resource settings, can limit fetal growth.
- Age and Parity: Extremes of maternal age (under 17 or over 35) and first-time pregnancies are associated with higher FGR risks.
2. Placental Factors
- Placental Insufficiency: The placenta may not develop properly or function adequately, leading to reduced blood flow and nutrient transfer.
- Placental Abruption: Premature separation of the placenta from the uterine wall can compromise fetal growth.
- Umbilical Cord Abnormalities: Issues like a single umbilical artery or cord compression can restrict nutrient delivery.
3. Fetal Factors
- Genetic Abnormalities: Chromosomal disorders like Down syndrome or Turner syndrome often result in FGR.
- Congenital Infections: Viral or bacterial infections during pregnancy can directly affect fetal development.
- Multiple Pregnancies: Twins or triplets are at higher risk of FGR due to shared placental resources.
Diagnosis of Fetal Growth Restriction
1. Clinical Assessment
- Fundal Height Measurement: A discrepancy between fundal height and gestational age may indicate FGR.
- Maternal Weight Gain: Poor maternal weight gain can be a red flag for FGR.
2. Ultrasound Imaging
- Estimated Fetal Weight (EFW): Ultrasound measures fetal head circumference, abdominal circumference, and femur length to estimate fetal weight.
- Amniotic Fluid Index (AFI): Low amniotic fluid levels often accompany FGR.
- Doppler Ultrasound: This assesses blood flow in the umbilical artery, middle cerebral artery, and ductus venosus, providing insights into placental function.
3. Biophysical Profile (BPP)
The BPP combines ultrasound and non-stress tests to evaluate fetal well-being. It assesses fetal movements, tone, breathing, and amniotic fluid volume.
4. Laboratory Tests
- Maternal Blood Tests: These can detect infections or conditions like preeclampsia that may contribute to FGR.
- Karyotyping: If genetic abnormalities are suspected, amniocentesis or chorionic villus sampling may be performed.
Management of Fetal Growth Restriction
1. Monitoring and Surveillance
- Frequent Ultrasounds: Regular ultrasounds track fetal growth and amniotic fluid levels.
- Doppler Studies: Serial Doppler assessments monitor placental blood flow and fetal well-being.
- Non-Stress Tests (NST): These evaluate fetal heart rate patterns to detect signs of distress.
2. Maternal Interventions
- Lifestyle Modifications: Encouraging smoking cessation, a balanced diet, and adequate rest can improve outcomes.
- Medications: In cases of preeclampsia or hypertension, antihypertensive drugs may be prescribed.
- Antenatal Corticosteroids: If preterm delivery is anticipated, corticosteroids can accelerate fetal lung maturation.
3. Timing of Delivery
Deciding when to deliver a growth-restricted fetus is a critical aspect of management. The goal is to balance the risks of prematurity against the risks of continued intrauterine stress.
- Early Delivery: If severe FGR or fetal distress is detected, early delivery may be necessary.
- Expectant Management: In mild cases, close monitoring may allow for continued intrauterine growth until term.
Outcomes of Fetal Growth Restriction
1. Short-Term Outcomes
- Perinatal Mortality: FGR significantly increases the risk of stillbirth and neonatal death.
- Birth Asphyxia: Poor placental function can lead to oxygen deprivation during delivery.
- Hypoglycemia: Growth-restricted infants often have low blood sugar levels after birth.
- Hypothermia: These babies may struggle to maintain body temperature due to low fat stores.
2. Long-Term Outcomes
- Neurodevelopmental Delays: FGR is associated with an increased risk of cognitive and motor impairments.
- Metabolic Syndrome: These children are more likely to develop obesity, diabetes, and cardiovascular diseases later in life.
- Growth Deficits: Some children may continue to experience growth delays into adulthood.
3. Maternal Outcomes
- Psychological Impact: Mothers of growth-restricted infants may experience anxiety, depression, or guilt.
- Future Pregnancy Risks: Women with a history of FGR are at higher risk for recurrence in subsequent pregnancies.
Prevention of Fetal Growth Restriction
1. Preconception Care
- Health Optimization: Managing chronic conditions like diabetes and hypertension before pregnancy can improve outcomes.
- Nutritional Support: Ensuring adequate intake of folic acid, iron, and other essential nutrients is crucial.
2. Antenatal Care
- Regular Check-Ups: Early and consistent prenatal care allows for timely detection and management of FGR.
- Lifestyle Counseling: Educating mothers about the risks of smoking, alcohol, and poor nutrition can prevent FGR.
3. Advanced Monitoring
High-Risk Pregnancy Care: Women with risk factors for FGR should receive specialized care, including frequent ultrasounds and Doppler studies.Contact Us
Conclusion
Fetal growth restriction is a complex and multifactorial condition that requires early diagnosis, careful monitoring, and tailored management. By understanding the causes, diagnostic methods, and treatment options, healthcare providers can improve outcomes for both mother and baby. For expectant parents, awareness of FGR and adherence to prenatal care recommendations are essential steps toward ensuring a healthy pregnancy.Schedule your Consultation with Dr. Ritesh Nawkhare
