Pelvic pain
Pelvic pain is a common yet often misunderstood condition that affects millions of people worldwide. Whether it’s a sharp, stabbing sensation or a dull, persistent ache, pelvic pain can significantly impact your quality of life. In this comprehensive guide, we’ll explore the causes, symptoms, and treatment options for pelvic pain, providing you with the knowledge you need to take control of your health.
What is Pelvic Pain?
Pelvic pain refers to discomfort in the lower abdomen, below the belly button, and between the hips. It can be acute, lasting for a short period, or chronic, persisting for six months or longer. Additionally, pelvic pain can vary in intensity, ranging from mild to severe, and may be constant or intermittent.
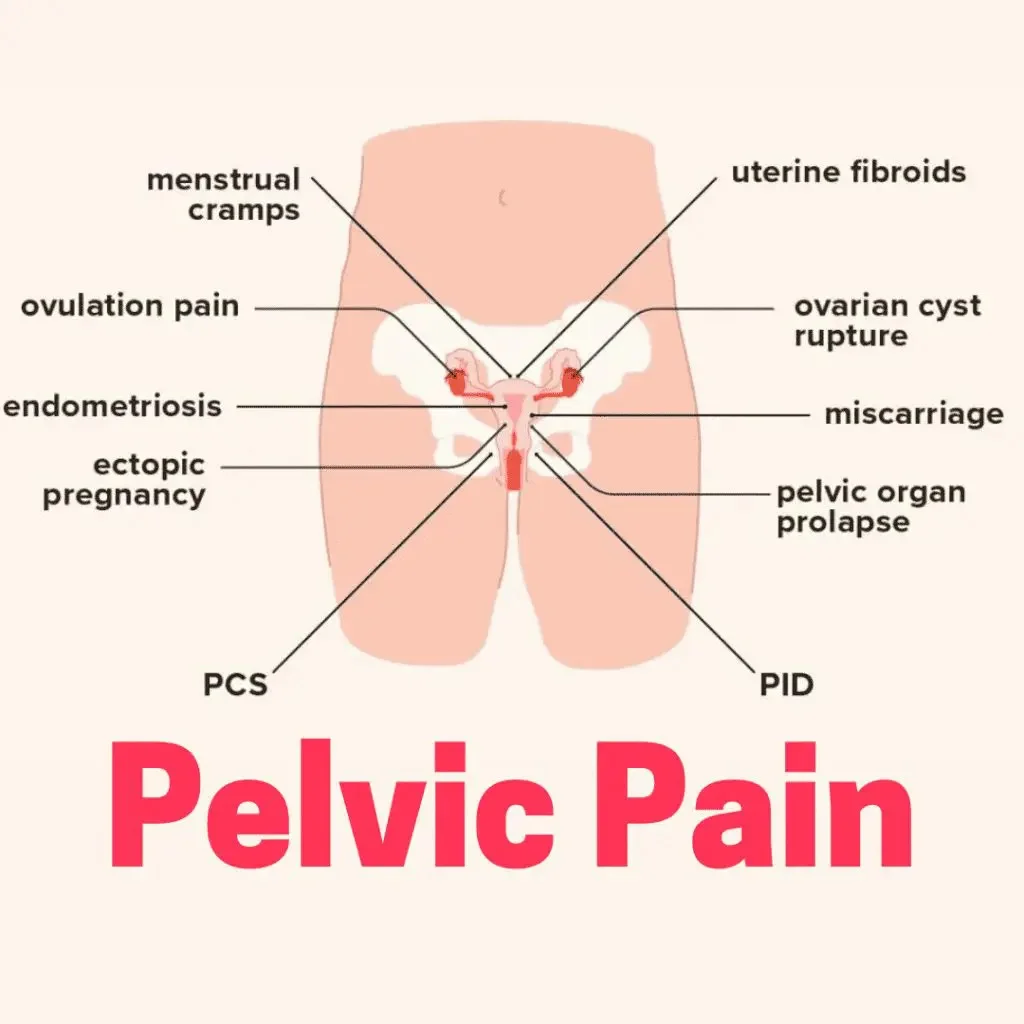
Common Causes of Pelvic Pain
Gynecological Issues
Many cases of pelvic pain are linked to the reproductive system. Conditions such as endometriosis, ovarian cysts, uterine fibroids, and pelvic inflammatory disease (PID) are frequent culprits. For instance, endometriosis occurs when tissue similar to the lining of the uterus grows outside the uterus, causing inflammation and pain.
Urinary Tract Disorders
Problems with the urinary system, such as urinary tract infections (UTIs), bladder infections, or interstitial cystitis, can also lead to pelvic pain. These conditions often cause a burning sensation during urination and frequent urges to urinate.
Gastrointestinal Problems
Disorders of the digestive system, including irritable bowel syndrome (IBS), constipation, and diverticulitis, can manifest as pelvic pain. IBS, in particular, is known for causing cramping, bloating, and discomfort in the pelvic region.
Musculoskeletal Issues
ometimes, pelvic pain stems from problems with the muscles, ligaments, or joints in the pelvic area. Conditions like pelvic floor dysfunction or muscle spasms can create significant discomfort.
Nerve-Related Pain
ometimes, pelvic pain stems from problems with the muscles, ligaments, or joints in the pelvic area. Conditions like pelvic floor dysfunction or muscle spasms can create significant discomfort.
Pregnancy-Related Causes
During pregnancy, the body undergoes numerous changes that can lead to pelvic pain. Round ligament pain, for example, is a common complaint among pregnant women and is caused by the stretching of ligaments that support the uterus.
Symptoms Associated with Pelvic Pain
- Menstrual Irregularities: Heavy or painful periods, spotting between periods, or irregular cycles may indicate a gynecological issue.
- Urinary Symptoms: Frequent urination, pain during urination, or blood in the urine can signal a urinary tract disorder.
- Digestive Issues: Bloating, diarrhea, constipation, or nausea may point to a gastrointestinal problem.
- Sexual Dysfunction: Pain during intercourse, also known as dyspareunia, is often associated with pelvic pain.
- Lower Back Pain: Many individuals with pelvic pain also experience discomfort in the lower back.
Diagnosing Pelvic Pain
- Medical History: Your doctor will ask about your symptoms, their duration, and any factors that exacerbate or alleviate the pain.
- Physical Examination: A pelvic exam may be performed to check for abnormalities in the reproductive organs, muscles, or nerves.
- Imaging Tests: Ultrasound, MRI, or CT scans can provide detailed images of the pelvic region, helping to identify structural issues.
- Laboratory Tests: Blood tests, urine tests, or cultures may be ordered to check for infections or other abnormalities.
- Minimally Invasive Procedures: In some cases, a laparoscopy may be necessary to directly visualize the pelvic organs and tissues.
Treatment Options for Pelvic Pain
Medications
- Pain Relievers: Over-the-counter pain relievers like ibuprofen or acetaminophen can help manage mild to moderate pain.
- Hormonal Therapies: For gynecological conditions like endometriosis, hormonal treatments such as birth control pills or GnRH agonists may be prescribed.
- Antibiotics: If an infection is causing the pain, antibiotics will be necessary to clear the infection.
- Muscle Relaxants: These can be helpful for pain caused by muscle spasms or tension.
Physical Therapy
Pelvic floor physical therapy is often recommended for individuals with musculoskeletal or nerve-related pelvic pain. A trained therapist can guide you through exercises to strengthen and relax the pelvic muscles.
Lifestyle Modifications
Making certain changes to your daily routine can alleviate pelvic pain. For example, maintaining a healthy diet, staying hydrated, and practicing stress-reduction techniques like yoga or meditation can be beneficial.
Surgical Interventions
In cases where structural abnormalities are causing the pain, surgery may be necessary. Procedures like laparoscopy for endometriosis or hysterectomy for severe uterine fibroids can provide relief.
Alternative Therapies
Some individuals find relief through alternative treatments such as acupuncture, chiropractic care, or herbal remedies. While these methods may not work for everyone, they are worth considering as part of a comprehensive treatment plan.
Preventing Pelvic Pain
- Maintain a Healthy Lifestyle: Eating a balanced diet, exercising regularly, and avoiding smoking can help prevent many conditions that cause pelvic pain.
- Practice Safe Sex: Using protection during sexual activity can reduce the risk of sexually transmitted infections that may lead to pelvic inflammatory disease.
- Stay Hydrated: Drinking plenty of water can help prevent urinary tract infections and constipation.
- Manage Stress: Chronic stress can exacerbate pain, so finding healthy ways to manage stress is essential.
When to Seek Medical Attention
- Unusual Vaginal Bleeding: Heavy bleeding, spotting between periods, or postmenopausal bleeding should be evaluated.
- Severe Pain: Pain that is sudden, intense, or accompanied by fever, nausea, or vomiting may indicate a serious condition.
- Difficulty Urinating: Inability to urinate, blood in the urine, or severe pain during urination requires immediate attention.
- Pregnancy-Related Pain: If you’re pregnant and experiencing pelvic pain, contact your healthcare provider to rule out complications.
Living with Pelvic Pain
- Educate Yourself: Knowing about your condition may enable you to make wise decisions regarding your treatment.
- Join a Support Group: Sharing with people who understand may give you emotional support and firsthand advice.
- Speak with Your Healthcare Provider: Keep the communication open with your doctor so that your treatment plan will be effective.
- Practice Self-Care: Prioritize relaxing and feel-good activities that make you unwind, such as soaking in a warm bath, meditating on mindfulness, or indulging in hobbies.Contact Us
Conclusion
Pelvic pain is a complex condition with a wide range of potential causes and treatments. By understanding the underlying factors and seeking appropriate medical care, you can take steps toward alleviating your discomfort and improving your quality of life. Remember, you don’t have to face pelvic pain alone—reach out to healthcare professionals, support groups, and loved ones for the help and support you need..Schedule your Consultation with Dr. Ritesh Nawkhare
