Placental disorders
Types of Placental Disorders
1. Placenta Previa
- Abnormal implantation of the fertilized egg
- Scarring of the uterine lining from previous surgeries or infections
- Multiple pregnancies
- Painless vaginal bleeding during second and third trimester
- Bright red bleeding
- Uterine contractions
- Ultrasound imaging
- Physical examination
- Bed rest
- Avoidance of strenuous activities
- Cesarean delivery if bleeding is severe
2. Placental Abruption
- High blood pressure
- Trauma to the abdomen
- Smoking or drug use during pregnancy
- Multiple pregnancies
- Vaginal bleeding
- Abdominal pain
- Uterine tenderness
- Rapid uterine contractions
- Ultrasound
- Physical examination
- Blood tests
- Immediate medical attention
- Hospitalization for monitoring
- Early delivery if necessary
3. Placenta Accreta
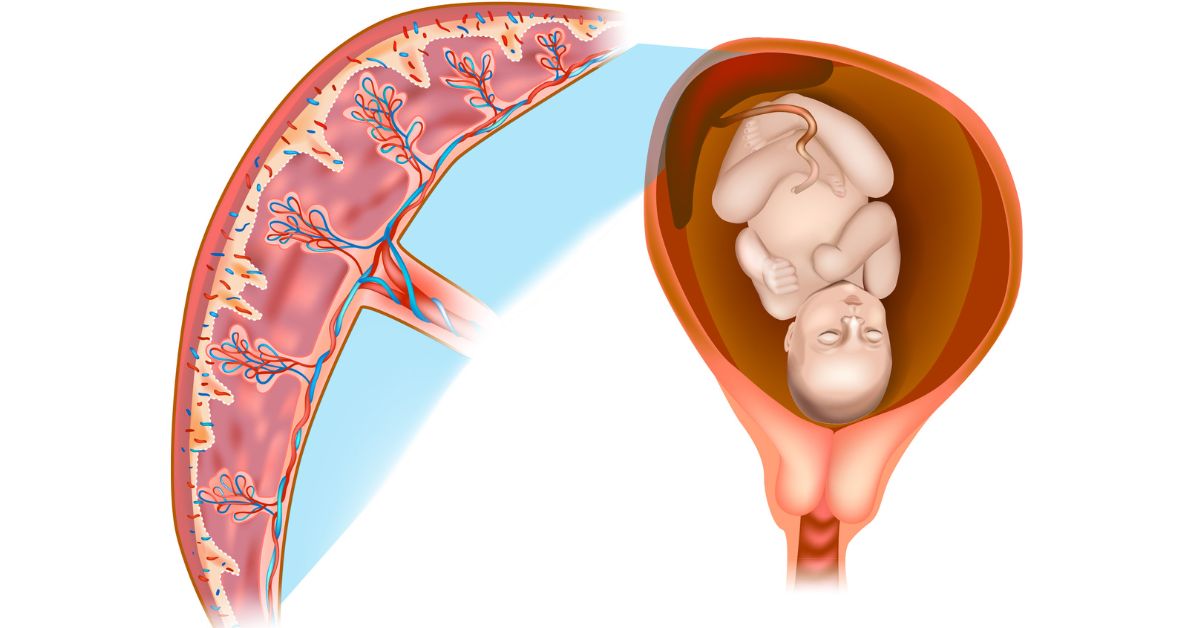
Placenta accreta is condition in which placenta grows too deeply into uterine wall. This can cause excessive bleeding during delivery and can necessitate surgery.
- Previous cesarean sections
- Uterine surgeries
- Advanced maternal age
- Often asymptomatic during pregnancy
- Severe bleeding during delivery
- Ultrasound
- MRI
- Planned cesarean section
- Hysterectomy in severe cases
4. Retained Placenta
Retained placenta is when the placenta is not expelled within 30 minutes of delivery. It can result in infection and excessive bleeding.
- Uterine atony (lack of uterine muscle tone)
- Abnormal placental attachment
- Previous retained placenta
- Heavy bleeding after delivery
- Fever
- Foul-smelling discharge
- Physical examination
- Ultrasound
- Manual removal of the placenta
- Medications to stimulate uterine contractions
- Surgery if necessary
5. Placental Insufficiency
Placental insufficiency refers to a situation in which the placenta is not functioning properly, resulting in inadequate fetal growth and development.
- High blood pressure
- Diabetes
- Smoking or drug use
- Multiple pregnancies
- Reduced fetal movement
- Small for gestational age baby
- Low amniotic fluid levels
- Ultrasound
- Doppler flow studies
- Non-stress test
- Close monitoring of the baby
- Early delivery if necessary
- Medications to improve blood flow
Causes of Placental Disorders
1. Maternal Health Conditions
- High Blood Pressure: Pregnancy-induced hypertension or chronic hypertension may impair placental function.
- Diabetes: Gestational or pre-existing diabetes may cause placental complications.
- Infections: Infections like chorioamnionitis may inflame the placenta and thus impair its function.
2. Lifestyle Factors
- Smoking: Pregnancy smoking may cut off blood supply to the placenta, resulting in complications.
- Drug Use: Illegal drug use may disrupt placental development and function.
- Poor Nutrition: Poor maternal nutrition may influence placental function and fetal growth.
3. Uterine and Placental Abnormalities
- Uterine Scarring: History of previous surgeries or cesarean deliveries may cause abnormal placental implantation.
- Multiple Pregnancies: Having more than one fetus may raise the risk of placental pathology.
- Advanced Maternal Age: Women aged above 35 are at increased risk of placental disorders.
Symptoms of Placental Disorders
- Vaginal Bleeding: One of the most frequent symptoms of placental disorders, particularly in placenta previa and abruption.
- Abdominal Pain: Abdominal or back pain may be a sign of placental abruption or complications.
- Decreased Fetal Movement: Decreased movement of the baby may be an indication of placental insufficiency.
- Uterine Contractions: Painful or frequent contractions can be an indicator of placental problems.
- Fever or Infection: Infection symptoms, like fever or smoldering discharge, can be an indication of a retained placenta or other complications.
Diagnosing Placental Disorders
- Ultrasound: The most frequent diagnosis of placental disorders is performed using ultrasound imaging. It enables healthcare professionals to see the location, size, and attachment of the placenta.
- MRI: MRI gives detailed pictures of the placenta and structures around it and aids in diagnosing conditions such as placenta accreta.
- Blood Tests: Blood tests can pick up evidence of infection, anemia, or other disorders that can influence the health of the placenta.
- Physical Examination: A complete physical examination, including a pelvic exam, may reveal evidence of placental disorders.
- Non-Stress Test: A non-stress test tracks the baby’s heart rate and movement, giving information about placental function.
Treatment Options for Placental Disorders
- Corticosteroids: Given to hasten fetal lung development in preterm delivery.
- Tocolytics: Drugs used to retard preterm labor.
- Antibiotics: Used to treat or prophylactically prevent infection.
2. Bed Rest
For placenta previa or mild placental abruption, bed rest is prescribed to avoid hemorrhage.
3. Hospitalization
Placental disorders can be so severe that they warrant hospitalization to be under careful observation and care.
4. Early Delivery
If the placental abnormality risks the mother’s or baby’s life, the baby might have to be delivered early by cesarean section.
5. Surgical Intervention
Surgical treatment, like a hysterectomy, may be indicated in cases of placenta accreta or retained placenta.Contact Us
Conclusion
Placental disorders are serious conditions that can have significant implications for both the mother and the baby. Understanding the types, causes, symptoms, and treatment options is crucial for managing these disorders effectively. Regular prenatal care, a healthy lifestyle, and early intervention can help reduce the risks and ensure a healthier pregnancy outcome. If you suspect any issues with your placenta, seek immediate medical attention to protect both your health and your baby’s well-being.Schedule your Consultation with Dr. Ritesh Nawkhare
