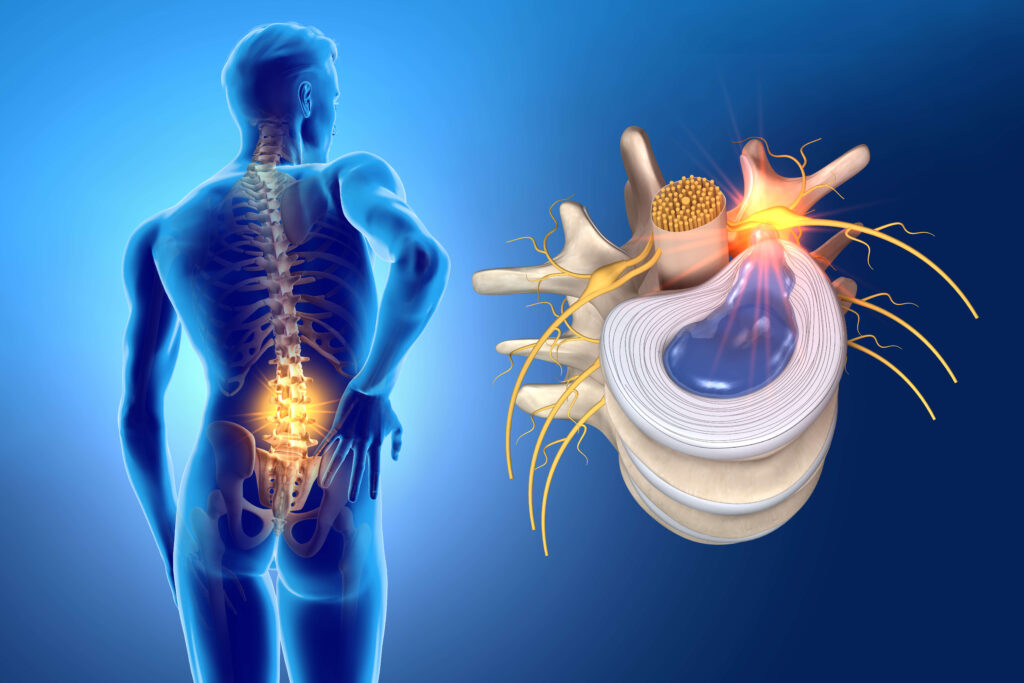
Disc herniation
What is Disc Herniation?
Causes of Disc Herniation
Disc herniation is often the result of a combination of factors, such as:
- Aging: As people age, the discs in their spine naturally lose water content, making them less flexible and more prone to tearing or rupturing.
- Trauma or Injury: Sudden accidents, such as falls, car accidents, or heavy lifting, can cause a disc to herniate by putting excessive pressure on the spine.
- Repetitive Strain: Repeated movements or poor posture over time can increase stress on the spine, leading to disc degeneration and eventual herniation.
- Genetics: Some people are genetically predisposed to disc herniation due to factors like spinal structure or inherited weaknesses in the discs.
Symptoms of Disc Herniation
The symptoms of disc herniation can vary depending on the location of the herniated disc and the extent of nerve compression. The most common symptoms include:
- Back or Neck Pain: The most noticeable symptom of disc herniation is pain in the affected area, such as the lower back or neck. This pain may be sharp or dull and can worsen with movement, bending, or twisting.
- Radiating Pain (Sciatica): When a disc herniates in the lower back, it can press on the sciatic nerve, causing pain that radiates down the leg. This is known as sciatica, and it often includes tingling, numbness, or weakness in the leg.
- Arm or Shoulder Pain: A herniated disc in the cervical spine (neck) can result in pain that radiates down the arm, shoulder, or hand. This is commonly accompanied by weakness, numbness, or tingling sensations in the arms.
- Muscle Weakness: Nerve compression from a herniated disc can lead to muscle weakness in the affected area, making it difficult to perform everyday tasks like lifting, walking, or gripping objects.
- Loss of Reflexes: In some cases, a herniated disc can affect reflexes, leading to diminished or absent reflexes in the knees, ankles, or other areas.
While the procedure is generally performed on an outpatient basis, the entire process usually lasts less than an hour. Local anesthesia is used to numb the area, and in some cases, sedation is administered to ensure the patient remains comfortable throughout the procedure.
How is Disc Herniation Diagnosed?
If you suspect you have a disc herniation, it is essential to consult with a healthcare professional. They will typically begin with a physical examination to assess your symptoms, posture, and range of motion. In addition to a physical exam, your doctor may order one or more of the following diagnostic tests:
- X-rays: X-rays can help rule out other potential causes of back or neck pain, such as fractures or tumors.
- MRI (Magnetic Resonance Imaging): An MRI is one of the most effective imaging techniques for diagnosing disc herniation. It provides detailed images of the soft tissues, including the discs, and allows doctors to see the extent of the herniation and its effect on surrounding nerves.
- CT Scan: A CT scan can provide additional information if an MRI is not possible or if the doctor needs further clarification of the herniation.
- Electromyogram (EMG): This test measures electrical activity in the muscles and can help determine if nerve damage is present.
Treatment Options for Disc Herniation
The treatment for disc herniation depends on the severity of the condition, the symptoms, and the patient’s overall health. In many cases, conservative treatments are effective in relieving pain and improving function. However, some patients may require surgical intervention. Below are the primary treatment options:
1. Conservative Treatments
For many people with disc herniation, non-surgical treatments can provide significant relief:
- Rest and Activity Modification: Taking short periods of rest while avoiding activities that exacerbate pain can help reduce inflammation and provide time for the disc to heal. However, prolonged bed rest is not recommended, as movement is essential for healing.
- Physical Therapy: A physical therapist can guide you through exercises to strengthen the muscles around your spine and improve flexibility. This can help alleviate pressure on the herniated disc and reduce pain.
- Medications: Over-the-counter pain relievers, such as ibuprofen or acetaminophen, can help manage mild to moderate pain. If the pain is severe, prescription medications such as muscle relaxants or nerve pain medications may be prescribed.
- Epidural Steroid Injections: In some cases, doctors may recommend an epidural steroid injection to reduce inflammation and relieve pain. This is often done when other treatments have not provided sufficient relief.
2. Surgical Treatments
If conservative treatments fail and the symptoms persist or worsen, surgery may be considered. Surgical options for disc herniation include:
- Discectomy: This procedure involves removing the portion of the herniated disc that is pressing on the nerve. It is often done on an outpatient basis with a minimally invasive approach.
- Laminectomy: A laminectomy involves removing a portion of the bone (lamina) over the affected disc to create more space for the nerves.
- Spinal Fusion: In severe cases, spinal fusion may be necessary to stabilize the spine. This involves fusing two or more vertebrae together after the herniated disc is removed.
Prevention of Disc Herniation
While not all cases of disc herniation can be prevented, several lifestyle changes can reduce the risk:
- Maintain a Healthy Weight: Excess weight puts added pressure on the spine, increasing the risk of disc herniation.
- Exercise Regularly: Strengthening the muscles in your back and core can provide better support for your spine, reducing strain on the discs.
- Practice Proper Posture: Good posture helps distribute weight evenly across the spine, reducing the chances of disc degeneration.
- Avoid Heavy Lifting: When lifting heavy objects, always use proper techniques—bend at the knees, not the waist—to prevent unnecessary strain on the back..Contact Us
Conclusion
Disc herniation is a common spinal condition that can cause significant pain and discomfort. Understanding the causes, symptoms, and treatment options available can help you manage this condition effectively. While many people can find relief through non-surgical methods like physical therapy and medications, some may require surgical intervention if conservative treatments are not effective. If you are experiencing symptoms of disc herniation, it’s important to consult with a healthcare provider to determine the best course of action.Schedule your Consultation with Dr. Ritesh Nawkhare
